Keywords:
By Constanze Drechsel
Myasthenia gravis is an autoimmune disease affecting 14-20/100,000 people in the U.S.1 and 1-9/100,000 people in Europe.2 The sad truth is that most of those afflicted go undiagnosed. Myasthenia gravis causes severe muscle weakness and significantly decreases quality of life. Diagnosis can be difficult, but state-of-the-art disease biomarkers and targeted assays are available to increase the likelihood that a patient with myasthenia gravis will be diagnosed early and can be treated appropriately. How can these biomarkers and use of the correct assays also help clinicians monitor therapeutic efficacy and support better treatment outcomes for their patients?
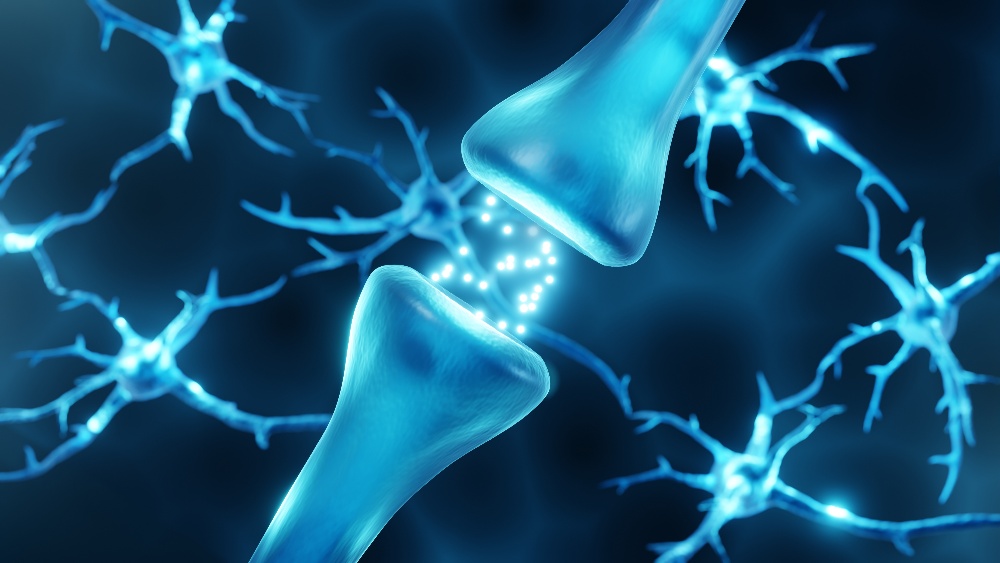
Myasthenia gravis causes muscle weakness when autoantibodies against acetylcholine or muscle-specific receptor tyrosine kinase block transmission of electrical signals from nerve endings to muscles.
Myasthenia gravis symptoms
In myasthenia gravis, the body’s own immune system produces antibodies that attack the skeletal muscles responsible for breathing and various other movements. This leads to patients experiencing muscle weakness and prolonged rest is needed to recover. There are effective treatments for myasthenia gravis3 but they are only effective if diagnosis is made early enough.
In most cases of myasthenia gravis, autoantibodies target acetylcholine receptors, which are essential for transmitting electrical impulses through muscle tissue. These electrical signals stimulate the muscles to contract. Acetylcholine receptor autoantibodies (ARAbs) produced in myasthenia gravis patients prevent acetylcholine from binding to its receptor which blocks normal muscle contractions.
Around 85% of people with myasthenia gravis have ARAbs, while the remaining 15% have so-called seronegative myasthenia gravis. Despite having clear clinical symptoms, these patients don't have detectable autoantibodies against the acetylcholine receptor. About half of these seronegative patients will instead have autoantibodies against a protein called muscle-specific tyrosine kinase (MuSK). MuSK plays an essential role in connecting the acetylcholine receptor to the muscles making it important in myasthenia gravis. Patients with MuSK autoantibodies typically have a more severe form of the disease, with more debilitating symptoms.
ARAb and MuSK account for 85-90% of myasthenia gravis diagnoses, meaning that even with good markers, there is no way to diagnose 10% of sufferers. One emerging marker that has shown diagnostic promise is the low-density lipoprotein receptor-related protein known as LRP4. One study tested patients who were seronegative for ARAb and MuSK for the presence of antibodies against LRP4. They discovered that 12 out of the 13 patients tested were positive for LRP4 making this one of the most promising markers to help close the gap on people suffering with undiagnosed myasthenia gravis.4
What makes myasthenia gravis diagnosis so complex?
ARAb and MuSK autoantibodies are the gold standard biomarkers for diagnosing myasthenia gravis. However, getting to that crucial early diagnosis is not simple. The first step is an assay for ARAbs, if Musk-Ab is not also measured right at the beginning. However, an ELISA for ARAbs is not sufficient, and is likely to yield a false positive result. To maximize the sensitivity and specificity of ARAb detection, a radioreceptor assay (RRA) is the preferred choice. The RRA is preferable because, unlike during an ELISA, the three-dimensional structure of the acetylcholine receptor is retained, which is essential for antibody recognition.
If the RRA test for ARAbs is positive, it aids in the diagnosis of myasthenia gravis. However, if the result is negative, it is important to consider the possibility of seronegative myasthenia gravis, which affects around 15% of patients. To identify these cases, a follow-up test with a MuSK ELISA is necessary, as it can detect around 50% of these patients. Due to this reason, more and more laboratories directly involve the measurement of Musk antibodies in the first line diagnostic. The preferred test for this follow-up is a quantitative MuSK ELISA, which is highly accurate and reliable, as we will explain below.
It also follows that if the test for MuSK is negative, then LRP4 could be the target. However, as there are no commercial tests currently available, laboratories would currently have to develop in-house assays which is now very time consuming under the In Vitro Diagnostic Regulation (IVDR). In such cases, it is probably best to collaborate with a commercial partner to get new test registered under IVDR and commercially available as soon as possible.4
A quantitative MuSK-Ab assay enables therapeutic monitoring
Patients with MuSK autoantibodies not only have a more severe form of the disease, but the therapy they receive also tends to be more aggressive, commonly involving rituximab immunosuppression to achieve B-cell depletion. In the treatment of myasthenia gravis, the target reduction of ARAbs is 50%, whereas the clinical goal of treatment in MuSK-positive patients is complete elimination of the MuSK autoantibodies. Calculating when this has been achieved requires a highly sensitive and quantitative assay, rather than relying on qualitative results.
Additionally, since therapy may require some time to take effect, by using a sensitive, quantitative assay, clinicians can carefully monitor the efficacy of myasthenia gravis treatment. They can detect increases or decreases in MuSK autoantibody levels and modify both treatment and therapeutic decision-making as needed.
Thankfully, both of these tests, ARAb and Musk-Ab, are available commercially under the IVDR and there will be a reliable supply going into the future. This is especially important in cases where rapid diagnosis is essential, which is the case with myasthenia gravis. Maastricht University Medical Center in The Netherlands uses an effective diagnostic protocol for myasthenia gravis, known as the ‘LAB Maastricht approach’. They have a particular focus on myasthenia gravis clinical practice and research, including an advanced therapeutic program. Their diagnostic method involves using an RRA to detect ARAbs, followed by quantitative MuSK-Ab ELISA for accurate diagnosis. This approach has proven to be successful in identifying cases of myasthenia gravis.
Are you using state-of-the-art assays and biomarkers for myasthenia gravis detection and treatment monitoring? For more information about our Myasthenia Gravis assays portfolio visit:

References
1. Myasthenia Gravis Foundation of America.
2. The Portal for Rare Diseases and Orphan Drugs.
3. National Institute of Neurological Disorders and Stroke. National Institutes of Health. Myasthenia Gravis.
4. Pevzner A, Schoser B, Peters K, Cosma NC, Karakatsani A, Schalke B, Melms A, Kröger S. Anti-LRP4 autoantibodies in AChR- and MuSK-antibody-negative myasthenia gravis. J Neurol. 2012 Mar;259(3):427-35. doi: 10.1007/s00415-011-6194-7. Epub 2011 Aug 5. PMID: 21814823.
Keywords:
About the author

Constanze Drechsel
Dr. Constanze Drechsel joined Tecan in 2019 as a product manager responsible for the autoimmunity and infectious disease portfolio. Constanze has a scientific background and completed her PhD research in protein and allergy chemistry and now supports the Global Reagent Marketing & Support department with immunoassay solutions at Tecan.










