Rheumatoid arthritis, type 1 diabetes and celiac disease are familiar examples of autoimmune disorders that occur when the immune system attacks healthy cells or tissues by mistake. Myasthenia gravis is a far rarer autoimmune disease, causing weakness in the skeletal muscles. LAB Maastricht UMC+ in the Netherlands has a long history with myasthenia gravis, using gold standard immunoassays to enable accurate diagnosis and provide the information necessary to allow effective treatment.
LAB Maastricht is the amalgamation of eight diagnostic functions at the Maastricht University Medical Center (MUMC+), including the central diagnostics lab, pathology, medical microbiology and clinical genetics. Its 1,000-strong team of laboratory specialists, clinicians, scientists and technicians offers a broad range of routine and specialist diagnostic services, as well as performing validation of new methods and supporting clinical trials.
Dr Jan Damoiseaux is a laboratory specialist in medical immunology at LAB Maastricht UMC+, and has specialized in autoantibody diagnostics since 1999. He explained: “After my PhD and a couple of years in immunology research, I was offered a three-year training program here at MUMC+, covering all aspects of laboratory investigations for autoimmunity, immunodeficiency, allergy, transplantation immunology and malignancies of the immune system. I am now responsible for autoimmune diagnostics in the lab – as well as teaching medical students and clinical trainees – and my research on autoantibody detection systems is very much linked to my clinical responsibilities.”
“Being a university hospital, we offer a broad spectrum of assays, with around 70-80 % of patient samples coming from our own hospital, and the rest from other regional hospitals and primary care. The lab has a central area for routine testing, supported by technology-based satellite labs – such as flow cytometry, protein electrophoresis and advanced immunodiagnostics – for specialist testing.”
Jan continued: “We have a special interest in myasthenia gravis (MG) here at MUMC+ in terms of both clinical practice and research, including a robotic thymectomy surgery program that was established after it was shown that the thymus is involved in the production of autoimmune antibodies, and its removal may be beneficial to MG patients. We therefore have a large number of MG patients who come to us for investigations, and it is vital that we accurately diagnose their condition through laboratory testing.”
Around 85 % of patients with clinical symptoms of MG are positive for autoantibodies to acetylcholine receptors, a transmembrane protein present in muscle cells. Radioreceptor assays (RRA) are the preferred lab tests for the detection of acetylcholine receptor autoantibodies (ARAbs) as, unlike ELISAs, these assays maintain the three-dimensional structure of the receptor that is essential for antibody recognition. “We originally trialed and validated the IBL International (Tecan) ARAb RRA on the recommendation of a clinician colleague specializing in MG,” Jan added. “This assay uses receptors from human muscle in combination with a radio-labeled alpha-bungarotoxin snake venom marker. The venom binds very specifically to acetylcholine receptors without interfering with ARAb binding, so there’s no need to purify the receptor. This is a very clever system, and the assay works very well, with good reproducibility and sensitivity. It’s also quantitative, which is particularly important for therapeutic monitoring. Our neurologists aim for a 50 % reduction in a patient’s ARAb levels after treatment with immunosuppressants. These therapies take time to work, and so ongoing monitoring of ARAb allows the treatment to be increased or changed if it is not having the desired effect.”
"Our previous experience with the company’s assays gave us confidence in its performance, so we didn’t look at any others."
For the 15 % of patients with clinical symptoms of MG but no detectable ARAbs – known as seronegative MG – it is now known that around 40 % have antibodies against muscle-specific kinase (MuSK), a protein involved in cross-linking the acetylcholine receptor to the cytoskeleton. Jan continued: “The discovery of MuSK autoantibodies is very important, because these patients have a more severe form of MG. Therapy is therefore more intensive, most commonly with rituximab immunosuppression to deplete B cells. Unlike the 50 % reduction target for ARAbs, the clinical aim for these patients is to completely eliminate anti-MuSK antibodies, making a sensitive assay vital. Some other laboratories in the Netherlands only report qualitative results, but we believe that it’s important to use a quantitative assay, allowing clinicians to review the efficacy of therapy. Tecan makes the only commercially-available quantitative anti-MuSK ELISA, and our previous experience with the company’s assays gave us confidence in its performance, so we didn’t look at any others.”

Kathleen Mallet, Veerle Mengels, Caroline Bijnens, Jos Wiersma and Jan Damoiseaux from the specialist immunology laboratory at MUMC+
“We have a good relationship with Tecan, and I’ve presented my work at several user meetings. I’ve also set up discussions for some of my research colleagues, who are looking at acetylcholine receptor blocking antibodies, and Tecan is keen to help with their research,” Jan concluded.
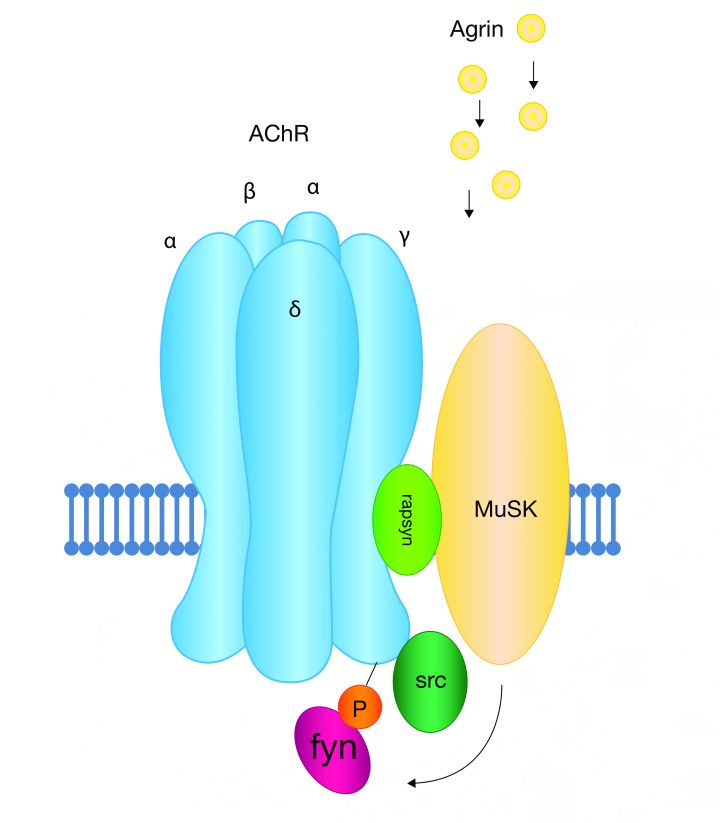
Agrin-induced clustering of acetylcholine receptors via MuSK
To find out more about IBL’s MG assays, visit www.tecan.com/immonoassays
To learn more about LAB Maastricht UMC+, go to www.labmaastricht.nl
Keywords:









