Keywords:
By Nastya Yeska
There is a definite role for IgG4 testing when diagnosing and treating pathologies that are associated with elevated levels of specific IgGs, such as Crohn’s disease, ulcerative colitis and irritable bowel syndrome.¹,² This is despite the fact that IgG4 testing has had a lot of bad press over the years, mainly because it has been shown that elevated IgG4 levels for certain food antigens may simply be an indicator of exposure and tolerance of a specific food, rather than an indicator of “true” food intolerance.³ With that in mind, we look here both at the science behind the tests, and the evolving IgG and IgG4 ELISA testing market.

Defining food intolerance
Individuals with allergies and other types of food sensitivities react adversely to certain foods and food ingredients that others can consume with no problems.
Allergies, such as reactions to specific proteins in wheat or milk, involve the immune system, and can be life-threatening. Symptoms usually appear within minutes of eating a problem food, and can include vomiting, facial swelling, rashes, or asthma-like symptoms. Food intolerances, on the other hand, tend to generate symptoms such as bloating or abdominal pain which are usually delayed, and can set in usually 24-72 hours after food intake, making it difficult to establish a causal relationship between the symptom and a specific food.
The mechanism of food intolerance is thought to occur through chronic stimulation of the gastrointestinal tract with certain food ingredients (food antigens), impairing its basic function, and potentially leading to chronic inflammation and greater permeability of the gut mucosa. This is what happens with irritable bowel syndrome (IBS), where concurrently, elevated serum IgG4 levels were reported towards specific foods in IBS patients.⁴⁵ Food elimination based on IgG4 levels improved symptoms in these individuals.⁶ More information and case studies can be found in this related article, which lends credence to testing in IBS patients.
The case for IgG4 testing in IBS
Depending on the diagnostic criteria employed, IBS affects around 11% of the population globally. About 30% of people who experience the symptoms of IBS end up consulting physicians for their IBS symptoms.⁷ IBS therefore constitutes a significant health care burden, and this burden is irrespective of setting or geography.⁷ The estimated global prevalence of IBS is shown in Figure 1.
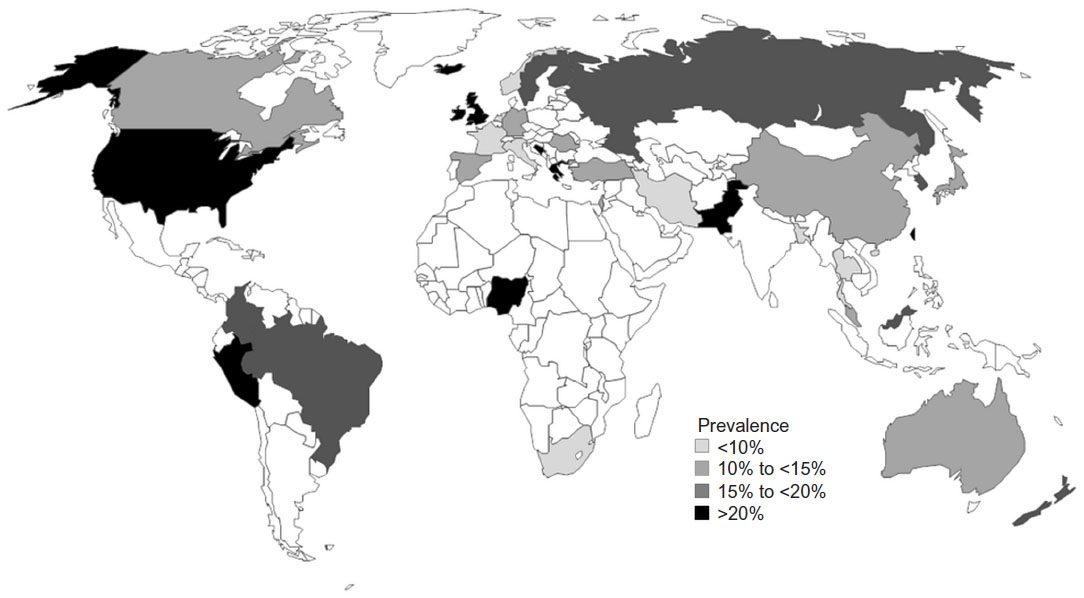
Figure 1: Worldwide prevalence of irritable bowel syndrome, as reported by country.⁷
However, accurate case definition remains difficult, due to the high frequency of symptoms within the community, variations in diagnostic criteria and the stringency with which they are implemented, lack of specific histopathological changes, and lack of a definitive point of onset globally.⁷
This is further complicated by the fact that patients with IBS are also more likely to already have or to develop other functional conditions, making epidemiological studies exceptionally challenging.⁷ The massive variation seen in IBS patients, and the sheer number of patients presenting with IBS symptoms who are consulting globally, suggests that if some form of standardized food intolerance IgG4 testing were to be implemented, this would be an extremely valuable addition to the clinical toolbox.
How does IgG4 testing fit into the food intolerance picture?
The gold standard for identifying food sensitivities is an elimination diet followed by an “oral challenge” of eating the eliminated foods one by one after a period of avoidance to determine the patient’s reaction, ideally without them knowing what’s being tested.¹⁰
To reduce the guesswork as to which foods are problematic, some practitioners will first ask for a food sensitivity or blood screening test to be carried out, such as an IgG4 ELISA test, to help guide the elimination diet. When a patient stops eating a problem food, they may have temporary withdrawal symptoms, so they might have to follow an elimination diet for about two weeks before these symptoms clear up and they are ready to start testing foods in an oral challenge. Following such an elimination diet requires dedication and commitment, as well as careful record-keeping.
Another area where food intolerance testing plays an essential role is in complementary medicine, where patients suffering from different chronic diseases other than those mentioned above are turning to holistic healthcare providers, frequently after conventional medicine has been unsuccessful. One such provider is RP Sanitas Humanus in the Netherlands. You can read here about how it is often found that food intolerances lie at the root of patients' chronic health issues and that this intolerance can be evaluated using automated analysis of IgG and IgG4 antibodies to isolate the true causes.
We see from the figures above that there are potentially around 250 million patients presenting with IBS symptoms who could be consulting globally at any one time, any or all of whom could benefit from IgG4 food intolerance testing.⁷ In addition, in 2019 there were almost 6.9 million people living with IBD (Crohn’s disease and ulcerative colitis) worldwide, with the number of prevalent cases is on the rise.¹¹ Add to this list the 1% of the global population likely to have celiac (coeliac) disease, and it is apparent that the development of a standardized form of IgG4 food intolerance testing would be advantageous.¹² So how can we best measure IgG and IgG4 levels?
Challenges in developing reliable food intolerance tests
Most of the kits that are commercially available for routine testing of IgG and IgG4 levels rely on immunological methods.⁸ ELISA methods are the most widely used, as they are sensitive and specific to detection of allergenic proteins and easy to use. However, there are many commercial kits for quantitative analysis available, which use different extraction buffers. Calibration procedures differ in the quality of the antibodies used, and the results vary among trademarks and batches. The major limitations include matrix effects, inadequate protein extraction, insufficient specificity due to cross-reactions and insufficient reproducibility of the results.⁹
With so many different IgG and IgG4-based food intolerance tests available, how can you be sure of choosing the ones that are right for your lab? Find out in the next article in our series, where you will read about five of the main challenges that need to be overcome if you want to develop a reliable food intolerance testing service.
References
- Lee, H. and Lee, K. J (2017). Alterations of Food-specific Serum IgG4 Titers to Common Food Antigens in Patients With Irritable Bowel Syndrome. Neurogastroenterol Motil, 23(4), 2093-0879. https://doi.org/10.5056/jnm17054
- Cai, C., Shen, J. et al. (2014). Serological investigation of food specific immunoglobulin G antibodies in patients with inflammatory bowel diseases. PloS one, 9(11), e112154. https://doi.org/10.1371/journal.pone.011215
- Gocki, J. and Bartuzi, Z. Role of immunoglobulin G antibodies in diagnosis of food allergy (2016) Postepy Dermatol Alergol. 2016 Aug; 33(4): 253–256. Published online 2016 Aug 16. doi: 10.5114/ada.2016.61600
- Bischoff, S.C., Barbara, G. et al. Intestinal permeability – a new target for disease prevention and therapy. BMC Gastroenterol. 2014; 14: 189. Published online 2014 Nov 18. doi: 10.1186/s12876-014-0189-7
- Zar S, Benson MJ, Kumar D. Food-specific serum IgG4 and IgE titers to common food antigens in irritable bowel syndrome. Am J Gastroenterol 2005;100:1550-1557.
- Zar S, Mincher L, Benson MJ, Kumar D. Food-specific IgG4 antibody-guided exclusion diet improves symptoms and rectal compliance in irritable bowel syndrome. Scand J Gastroenterol 2005;40:800-807.
- Canavan, C., West, J., & Card, T. (2014). The epidemiology of irritable bowel syndrome. Clinical epidemiology, 6, 71–80. https://doi.org/10.2147/CLEP.S40245
- Velikova, T., A Kukov, A. et al. (2018). Methods for detection of food intolerance. R Adv Food Sci: 1(3): 106-119 ISSN: 2601-5412 11
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2014. Scientific Opinion on the evaluation of allergenic foods and food ingredients for labelling purposes. EFSA Journal 2014;xx(xx):NNNN, 277 pp.doi:10.2903/j.efsa.2014.NNNN
- Vojdani, A. (2015) The evolution of food immune reactivity testing: why immunoglobulin G or immunoglobulin A antibody for food may not be reproducible from one lab to another. Altern Ther Health Med.;21 Suppl 1:8-22.
- Naghavi, M., Malekzadeh, R. et al., Lancet Gastroenterol Hepatol. 2020; 5: 17–30. Published Online October 21, 2019 https://doi.org/10.1016/S2468-1253(19)30333-4
- Green PH, Cellier C. Celiac disease. N Engl J Med. 2007;357:1731–1743
Keywords:
About the author

Nastya Yeska
Nastya Yeska joined Tecan in 2017 as a product manager responsible for the Complementary medicine product portfolio, including Food intolerance and Saliva diagnostics. Nastya is part of Global Reagent Marketing & Support Department responsible for delivering ELISA solutions. In 2021, she changed her role to Integrated Marketing Manager.