By Nicholas Smith
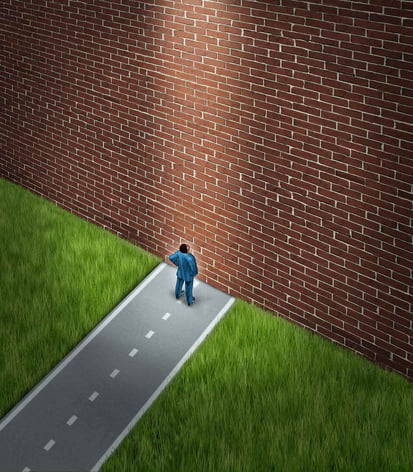
The intention by the U.S. Food and Drug Administration (FDA) to issue a new guidance that would bring oversight of laboratory developed tests (LDTs) directly under FDA regulatory control, instead of the current paradigm in which LDTs are regulated by FDA's Clinical Laboratory Improvement Amendments (CLIA), is creating much uncertainty and not a little distress. What would this significant change mean for laboratories that already rely on LDTs, are improving existing tests and actively developing new ones?
How could clinical laboratories possibly cope with the economic impact of more burdensome regulatory requirements for LDTs? If they can no longer offer the tests what effect would that have on the advancement of personalized medicine? According to Randy Prebula, Partner, Hogan Lovells, "Most premarket and post-market controls implemented in FDA regulation of LDTs would be inherently disruptive to all stakeholders in these industries: device manufacturers (IVDs, instruments, accessories, sample collection devices, RUO-labeled products); and clinical laboratories in all aspects of LDT development, verification, and performance."
Warning: Potential Impact of FDA Guidance
The proposed regulation of LDTs as medical devices by FDA is "a flawed approach," says Alan Mertz, president of the American Clinical Laboratory Association. The solution is not a CLIA-only approach, but rather legislation that creates " a new pathway through CLIA and FDA" and recognizes the important differences between LDTs and IVDs. New legislation should also consider the value of LDTs, the complexity of laboratory testing, and the potential for FDA regulatory oversight to slow the advancement of new diagnostic testing paradigms to support precision medicine, in Alan Mertz's view.
Andre Fish, Executive Director of AdvaMedDx describes a "widespread feeling that there is currently a lack of transparency and premarket assurance" of the clinical validity of CLIA-regulated tests. He emphasizes that "tests" (reagents, instruments, and systems) are distinct from "testing" and require analytical and clinical validity. AdvaMedDx encourages a risk-based approach to test regulation. "Ultimately this is about whether a test is going to work for a patient, and the risk is the same regardless of who has developed the test."
More Burdensome Regulatory Paradigm Would Slow the Path to Precision Medicine
Laboratories produce LDTs to fill gaps in testing, when a patient requires a test that is not available from a manufacturer of test kits and reagents. James Nichols, Chair, Government Affairs Committee of the American Association of Clinical Chemistry (AACC) cites a range of examples of LDTs, including the following:- Research-based tests transitioned to the clinical laboratory
- Colorimetric tests for metabolites
- Bleeding times for clotting disorders HPLC for drug and therapeutic monitoring
- Molecular testing for new strains of respiratory viruses (e.g., SARS or MERS) and emerging infections (Ebola) Lamellar body counts for fetal lung maturity
Assessing the current regulatory landscape, Mr. Nichols states, "Many analyzer platforms and sample handling devices are exempt [from premarket submission]. Some are also exempt from QSR compliance." However, if LDTs become included under the umbrella of FDA regulation, then "the need to seek clearance/approval, impact of CLIA complexity categorization, and the need to establish QSR control (at least for Design and Development) likely will change."If the FDA regulates LDTs as they do manufacturer-derived tests, they would have to undergo Premarket Review, with documentation of clinical validity, test limitations, and evidence provided that LDT performance meets Quality Systems Requirements (QSR).
Furthermore, ongoing post-market surveillance would be required, with notification of adverse events to the FDA. Clinical laboratories lack the funds and staff to produce this documentation, and requiring it would slow or prevent the translation of research findings to clinical medicine, according to Mr. Nichols. This "is contrary to where we are trying to go with laboratory medicine," he says. "Regulatory bodies should allow labs to establish clinical validity through a variety of ways -- literature, patient benefit, standard of care."
How can instrument manufacturers and clinical laboratories work together to prepare for impending regulatory changes and try to minimize the impact on their ability to develop and implement LDTs? "Key to managing this disruption in a positive way will be understanding, and anticipating and working effectively with FDA and stakeholders to make sure the framework is properly scoped, feasible, and not overly burdensome," says James Nichols.
Tecan's many years of experience working in the highly regulated IVD medical device market and our expertise in collaborating with researchers and clinicians to manufacture validated and compliant automated sample handling and detection systems allows us to help you navigate the uncertain regulatory future of LDTs. When you partner with Tecan, you benefit from access to a broad scope of knowledge and technological expertise, and a strong record of regulatory compliance in the development of diagnostic testing systems.
Contact Tecan to talk about LDTs, advancing personalized medicine, and how we can work together to make a difference for patients.
About the author

Nicholas Smith
Nicholas Smith is Head of Global Marketing and Portfolio Management for Tecan’s Partnering Business. A key function of his team is to work closely with customers to develop new product concepts and proposals based on a thorough analysis of their specific requirements. Nicholas’ joined Tecan in 2012 from Roche Diagnostics where he worked for over 20 years in a variety of roles within marketing and business development.











